- Home
- Breast Surgery
BREAST SURGERY
One of the most common questions during Dr. Reid’s breast augmentation patient consultations pertains to sizing. In general, there are key breast ratios that are universally considered attractive. During your breast implant selection and sizing with Dr. Reid, he will carefully assist you to ensure that these key ratios are corrected and/or maintained in order to create beautiful natural looking breasts that are balanced with respect to your individual body type.
The illustrations below (figures 1, 2 & 3) show how proper pre-operative measurement and respecting the importance of key ratios can lead to an optimum surgical outcome.
Before Surgery
Patients seek Dr. Reid’s breast augmentation surgery expertise to address a variety of reasons including:
-
- Enhancing breast shape
- Enlarging breasts for aesthetic reasons
- Breast reconstruction
Key Distances
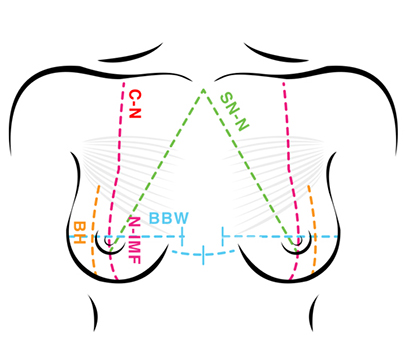
Key breast ratios—ensuring proportion and symmetry of these ratios are key to giving breasts a natural youthful look.
-
- BH - measures breast height
- BBW – measures base breast width
- N-IMF – measures the distance between nipple to inframammary fold
After Surgery
Careful execution of surgical plans ensures your new breasts look and feel as natural as possible by:
-
- Ensuring symmetry between breasts
- Maintaining and/or correcting key distances to ensure each breast is well proportioned

Financing with Beautifi
We have partnered with Beautifi to bring you industry leading interest rates and affordable monthly payment options. Beautifi is a specialized provider of plastic surgery and cosmetic procedure financing solutions. Beautifi offers affordable and flexible loans ranging from $1,500 – $25,000+. Scan the QR code below or click to apply.
Why wait? Get the procedure you want today!
- Flexible Payment Terms
- No Money Down Required
- No Pre-Payment Penalties
- No impact to your credit score
- Rates starting at 8.95%
- Terms from 6 months to 6 years

Dr. Owen Reid MD FRCSC
Education
Dr. Reid has trained specifically in plastic surgery. He completed medical school with honors at the University of British Columbia prior to receiving training in surgery of the breast and body.
Experience
Dr. Reid is an experienced, board-certified plastic surgeon. He frequently attends conferences relating to reconstructive and cosmetic surgery while maintaining an active interest in post-weight loss surgery.
Meet The Staff
The experienced team at Dr. Owen Reid’s plastic surgery center is committed to providing comprehensive, individualized care, the highest level of safety, and optimal results as they guide patients through their journey toward achieving their cosmetic goals.




